The below list highlights just some of the recent and ongoing projects driven by the Fischell Foundry. Additional projects will be shared as details can be made public.
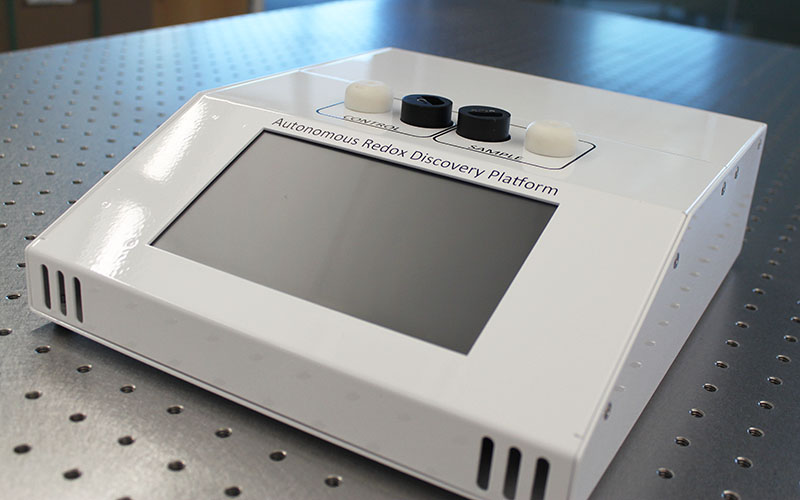 Fischell Institute faculty member Gregory Payne (Institute for Bioscience and Biotechnology Research) and a team of researchers developed a tool that detects biological signatures in blood that measures the level of oxidative stress in a patient. The standard techniques to measure oxidative stress in clinical samples generally involve measuring individual antioxidants, a costly, time-consuming process that can potentially miss important markers for diagnosing or treating diseases. Knowing this, the UMD research team’s method applies the power of signal processing to chemical analysis, enabling a rapid and adaptable diagnostic tool.
Fischell Institute faculty member Gregory Payne (Institute for Bioscience and Biotechnology Research) and a team of researchers developed a tool that detects biological signatures in blood that measures the level of oxidative stress in a patient. The standard techniques to measure oxidative stress in clinical samples generally involve measuring individual antioxidants, a costly, time-consuming process that can potentially miss important markers for diagnosing or treating diseases. Knowing this, the UMD research team’s method applies the power of signal processing to chemical analysis, enabling a rapid and adaptable diagnostic tool.
Along with Payne, Deanna Kelly, professor of psychiatry and affiliate professor of pharmacy practice and science at the University of Maryland School of Medicine; IBBR Post-Doctoral Associate Mijeong Kang; and IBBR Research Associate Eunkyoung Kim invented the device. Fischell Institute Chief Engineer John Rzasa executed the device design in-house. They first applied their technology to detect signatures of oxidative stress in people living with schizophrenia, but, more recently, they have worked on applications for cardiovascular disease and necrotizing enterocolitis in premature infants.
Fischell Foundry member Lex Schultheis and Fischell Institute director William Bentley are leading a series of biocompatibility studies on 3D-printed dental devices.
This research is part of a University of Maryland Center of Excellence in Regulatory Science (M-CERSI) project initiative aimed at informing FDA reviews regarding the likelihood that novel 3D printing methods of dental devices will cause adverse reactions in patients such as allergic, inflammatory, or toxicological reactions.
Past studies on 3D printers have shown that certain resins, when 3D printed, may be biocompatible for direct patient contact in dental procedures, particularly oral surgery.
A principal focus of the group's work will be evaluation of Form 2 Dental LT resin using a new stereolithography (SLA) printer workstation dedicated specifically for this research. Using a printer which has only been exposed to one resin type minimizes contamination and simplifies data interpretation.
The group plans to demonstrate 3D-printed parts that adhere to industry acceptance standards for biocompatibility as well as precise parameters of 3D printing and process control. If the device meets these standards, its development will also serve as a reference point for the creation of future biomedical devices.
Schultheis and Bentley are working with FDA collaborators James Coburn, Matthew Di Prima, Katherine Vorvolakos, Berk Oktem, Keaton Nahan, and Rakhi Dalal.
 Single-use N95 respirators – first developed by 3M – are different from standard surgical masks in that they are designed to filter up to 95% of airborne particles, such as viruses from the air. Even more, 3M respirators also apply an electrostatic charge to the material to further prevent incredibly small particles from making their way through the mask fibers. The longer a caregiver or patient wears the N95 respirator, the more likely it is that it will become ineffective. In addition, nurses wearing the same mask for lengthy hours have experienced significant facial bruising. Given this experience, N95-rated respirators that can be cleaned and safely reused are in high demand as hospitals and physician's offices worked through their supplies during the COVID-19 health crisis.
Single-use N95 respirators – first developed by 3M – are different from standard surgical masks in that they are designed to filter up to 95% of airborne particles, such as viruses from the air. Even more, 3M respirators also apply an electrostatic charge to the material to further prevent incredibly small particles from making their way through the mask fibers. The longer a caregiver or patient wears the N95 respirator, the more likely it is that it will become ineffective. In addition, nurses wearing the same mask for lengthy hours have experienced significant facial bruising. Given this experience, N95-rated respirators that can be cleaned and safely reused are in high demand as hospitals and physician's offices worked through their supplies during the COVID-19 health crisis.
To address this critical need, the Fischell Foundry has worked in close collaboration with clinicians, faculty, and staff across the University of Maryland, College Park (UMD) and Baltimore (UMB) campuses – as well as with Walter Reed National Military Medical Center, Washington Hospital Center, and Children's National Medical Center – to develop solutions that will keep both doctors and patients safe.
Fischell Institute director William E. Bentley, faculty member Lex Schultheis, M.D., Ph.D., and engineer Kevin Aroom led UMD's charge to develop a prototype of a reusable mask that can be personalized to fit the contours of an individual's face. With the help of input from other institutions and dozens of engineers – including UMD Unmanned Aircraft Systems Test Site Director Matthew Scassero – and clinicians – including UMB's Joseph R. Scalea, M.D. – Aroom logged long hours in the Fischell Institute lab working to design and test 3D-printed molds for conformal masks using facial scanning software and in-house printers, including those in Terrapin Works.
As testing confirms the safety and effectiveness of the Fischell Foundry's respirator, the hope is that the U.S. pipeline of N95 respirators could be bolstered by U.S. industry and maker facilities such as UMD's own Terrapin Works and ActivArmor, a long-time Fischell Institute collaborator that specializes in custom 3D-printed casts and splints.
Fischell Institute MPower fellow Quinn Burke is working to develop and enhance a conformal respirator mask alongside ActivArmor. His efforts center on testing the masks to meet FDA, the National Institute for Occupational Safety and Health (NIOSH), and Occupational Safety and Health Administration (OSHA) standards. One of Burke's goals is to scale up the manufacturing of these enhanced masks in Maryland.
The Fischell Institute filed for a U.S. Food and Drug Administration Emergency Use Authorization.
News highlights
The Firefly project is a collaboration with Fischell Institute faculty member Giuliano Scarcelli (Fischell Department of Bioengineering) and Amal Isaiah (University of Maryland School of Medicine). Firefly is a device that will be used to provide real-time intraocular pressure testing with greater accuracy than the current puff test method. Cameras positioned at eye level enable a more accurate assessment and quantification than the current method. Engineers at the Fischell Insittute are developing a prototype machine to provide pressure data to Drs. Scarcelli and Isaiah.
 As testing for COVID-19 ramped up across the country, the safety of medical personnel who administer the tests became a high-priority concern, particularly at pop-up testing sites assembled in public spaces.
As testing for COVID-19 ramped up across the country, the safety of medical personnel who administer the tests became a high-priority concern, particularly at pop-up testing sites assembled in public spaces.
Recognizing this, researchers at the University of Maryland Robert E. Fischell Institute for Biomedical Devices worked in collaboration with Johns Hopkins University and the Baltimore City Health Department to develop a low-cost, rapidly deployable mobile testing booth—similar to a traditional phone booth in both size and shape. The booth, made primarily of acrylic and aluminum, uses a HEPA filter blower to create a positive pressure system, whereby the air pressure inside the booth is higher than outside the booth. This protects the personnel administering the test by preventing virus particles and other germs from entering the booth. In this way, the booth creates a cleanroom environment similar to those commonly used in the pharmaceutical and medical device industries to test products and medical equipment without the threat of contaminants.
Extending from the front of the booth are gloves that allow the medical personnel inside to administer the test to someone outside the booth without making direct contact. The gloves are of a specialized, chemical-resistant grade, which makes them sturdy enough to withstand constant cleanings before each new patient.
For the testing procedure, the patient sits outside the booth in a chair seated next to the gloves. The medical personnel inside the booth uses the gloves to retrieve a testing swab from a tray mounted on the outside. He or she then uses an intercom system to ask the patient to tilt their head, before using the swab to collect a sample from the cavity between the patient’s nose and mouth. The medical personnel then collects the swab via a tray attached on the outside of the booth. Once the patient vacates the area, test site personnel thoroughly clean the gloves, chair, and front side of the booth. When the person inside the booth is ready to receive the next patient, he or she steps on a pneumatic switch to display a signal.
Johns Hopkins University assistant professor Axel Krieger and Fischell Institute senior engineer Kevin Aroom led the efforts to develop the first prototypes of the booth. The duo worked in close collaboration with mechanical engineering Ph.D. students Jiawei Ge and Lidia Al-Zogbi, both of whom studied in Krieger’s Medical Robotics and Equipment Lab.
Together, the team hopes their rapidly deployable testing booth could help ensure the safety of those working to administer COVID-19 tests—a need that is likely to grow in the coming weeks and months.
Recent News
Fischell Foundry member John Rzasa is part of the development team that designed a smart otoscope to quickly and accurately assist in the diagnosis of pediatric ear infections. The concept originated with Drs. Therese Canares and James Clark at Johns Hopkins University School of Medicine as a tool to accurately diagnose ear infections in children and thereby reduce antibiotic overuse – a major concern to parents and doctors.
The OtoPhoto team won a $20,000 grant from the National Capital Consortium for Pediatric Device Innovation (NCC-PDI) during its 2020 "Make Your Medical Device For Kids!" competition. NCC-PDI is a U.S. Food and Drug Administration (FDA)-funded collaboration between Children's National Hospital and the University of Maryland's Robert E. Fischell Institute for Biomedical Devices.
The medical innovation, dubbed a vehicle for “safer ear exams in a COVID-19 world” leverages machine learning technology, and is intended for home telehealth use.
The OtoPhoto team is working on clinical trials and next steps to bring the product to market.
Recent News
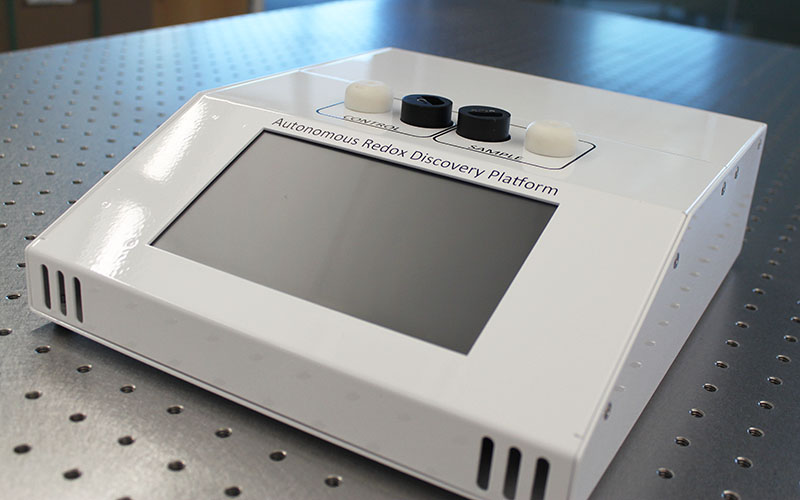 Fischell Institute faculty member Gregory Payne (Institute for Bioscience and Biotechnology Research) and a team of researchers developed a tool that detects biological signatures in blood that measures the level of oxidative stress in a patient. The standard techniques to measure oxidative stress in clinical samples generally involve measuring individual antioxidants, a costly, time-consuming process that can potentially miss important markers for diagnosing or treating diseases. Knowing this, the UMD research team’s method applies the power of signal processing to chemical analysis, enabling a rapid and adaptable diagnostic tool.
Fischell Institute faculty member Gregory Payne (Institute for Bioscience and Biotechnology Research) and a team of researchers developed a tool that detects biological signatures in blood that measures the level of oxidative stress in a patient. The standard techniques to measure oxidative stress in clinical samples generally involve measuring individual antioxidants, a costly, time-consuming process that can potentially miss important markers for diagnosing or treating diseases. Knowing this, the UMD research team’s method applies the power of signal processing to chemical analysis, enabling a rapid and adaptable diagnostic tool.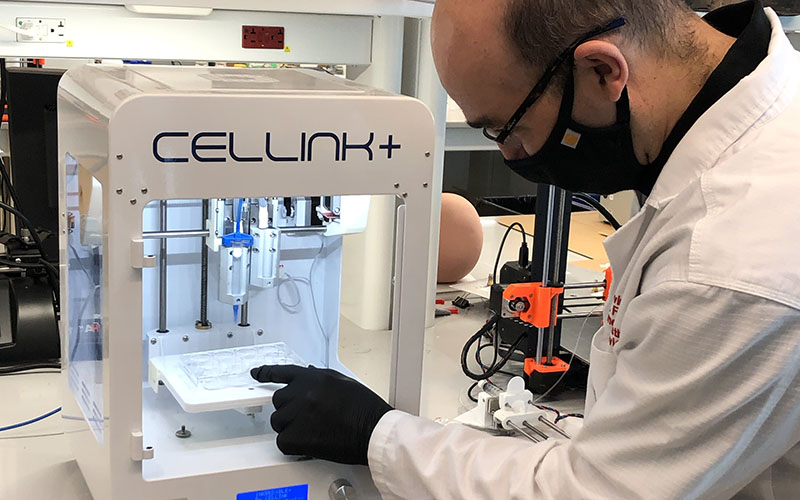
 Single-use N95 respirators – first developed by 3M – are different from standard surgical masks in that they are designed to filter up to 95% of airborne particles, such as viruses from the air. Even more, 3M respirators also apply an electrostatic charge to the material to further prevent incredibly small particles from making their way through the mask fibers. The longer a caregiver or patient wears the N95 respirator, the more likely it is that it will become ineffective. In addition, nurses wearing the same mask for lengthy hours have experienced significant facial bruising. Given this experience, N95-rated respirators that can be cleaned and safely reused are in high demand as hospitals and physician's offices worked through their supplies during the COVID-19 health crisis.
Single-use N95 respirators – first developed by 3M – are different from standard surgical masks in that they are designed to filter up to 95% of airborne particles, such as viruses from the air. Even more, 3M respirators also apply an electrostatic charge to the material to further prevent incredibly small particles from making their way through the mask fibers. The longer a caregiver or patient wears the N95 respirator, the more likely it is that it will become ineffective. In addition, nurses wearing the same mask for lengthy hours have experienced significant facial bruising. Given this experience, N95-rated respirators that can be cleaned and safely reused are in high demand as hospitals and physician's offices worked through their supplies during the COVID-19 health crisis.  As testing for COVID-19 ramped up across the country, the safety of medical personnel who administer the tests became a high-priority concern, particularly at pop-up testing sites assembled in public spaces.
As testing for COVID-19 ramped up across the country, the safety of medical personnel who administer the tests became a high-priority concern, particularly at pop-up testing sites assembled in public spaces.