News Story
Jewell Awarded $1.4 Million NIH Grant for Novel Multiple Sclerosis Research

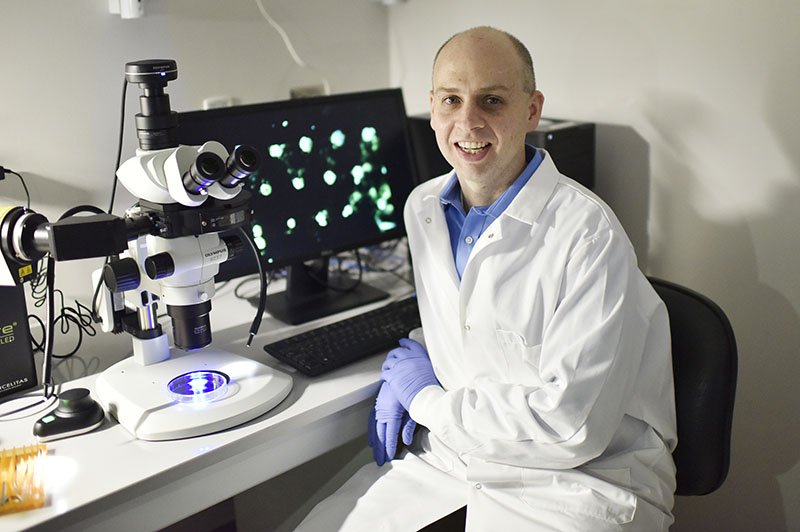
Dr. Chris Jewell
Fischell Department of Bioengineering (BIOE) Associate Professor Christopher Jewell was awarded a four-year, $1.4 million National Institutes of Health (NIH) Research Project Grant (R01) for his efforts to study the immunology behind autoimmune disease and develop new advanced therapies for diseases such as multiple sclerosis (MS).
Autoimmune disease causes the body to identify its own “self” cells as foreign and, in response, the immune system attacks healthy tissue. In MS, the immune system incorrectly recognizes components of the central nervous system, causing inflammation and destruction of myelin, the fatty substance that surrounds and protects nerve fibers. When this happens, nerve fibers and cells are damaged, leading to a loss of motor function and other complications.
To lessen the immune system’s attack against self cells, conventional therapies rely on general immune suppression – a strategy that has proven effective, but can leave patients susceptible to disease or infections.
To explore new pathways toward MS treatments that would leave the patient’s immune system intact, Jewell, his collaborator Dr. Jonathan Bromberg (University of Maryland School of Medicine Professor of Surgery and Microbiology and Immunology), and the rest of his team are using degradable biomaterials and combinations of immune signals to study how local changes to the function of lymph nodes – the tissues that determine how immune responses develop – could affect the body’s ability to defend against foreign invaders while inflicting minimal harm to itself.
This process, known as immunological tolerance, represents the bullseye for MS therapies.
“New technologies that allow selective tolerance could stop the mistaken attack of host tissue during autoimmunity without suppressing normal immune functions,” said Jewell, a member of the University of Maryland's Robert E. Fischell Institute for Biomedical Devices.
Several pre-clinical reports and clinical trials have indicated that co-administration of myelin peptide and tolerizing immune signals can promote the development of a special kind of immune cell, called regulatory T cells, which ameliorate disease.
While bioengineers understand that the lymph nodes determine whether or not a T cell becomes inflammatory, there is still little known about how signal integration in the lymph nodes drives immunological tolerance. New knowledge in this arena could help address limitations associated with current therapies, such as incomplete control of disease and non-specific immunosuppression, Jewell said.
To work towards next-generation therapies for MS, Jewell and his team are using a new platform that combines direct intra-lymph node injection with controlled-release biomaterial depots to observe the resulting impact on immunological tolerance.
Their work shows promise; preliminary data in mice have demonstrated that a single dose of these depots – which contain a myelin peptide and a drug known as rapamycin – permanently reverses disease-induced paralysis in a model of MS. Even more, these effects occur even when the biomaterial depots are administered at the peak of disease, confirming the power of this system to serve as a tool to locally control the function of one lymph node, while dissecting the impact on systemic tolerance and at distant sites such as the central nervous system and spleen.
"Direct lymph node delivery is a valuable tool to probe immune function because we can control the specific combinations and relative levels of signals in the lymph node,” Jewell said. :Additionally, since these tissues are locations where immune cells develop, controlling the local environment provides a new route to direct how immune cells develop – toward regulatory T cells, for example – that can then migrate out of the node into the body to selectively control disease.”
Jewell and his team hypothesize that their platform will advance understanding on the roles that local signals, combinations, and kinetics within lymph nodes play in programming the nature of immunological tolerance. Additionally, they believe that their work will also generate findings that inform the design of new therapies for other autoimmune diseases such as Type 1 diabetes and rheumatoid arthritis.
Published April 20, 2018