This well-established fellowship has helped students transition multiple medical device ideas into prototypes and commercial ventures while earning their Master of Engineering (M.Eng.) degrees.
The fellowship is open to students graduating from engineering, pharmacy, or related STEM programs.
Application requirements include your: Resume, Statement of Purpose, Business Plan, Transcript, and Two letters of Recommendations
Please note that there is no maximum or minimum word count for the statement of purpose or business plan.
Business plans should answer the following:
Applicants who do not have a current project or product for which they would like to submit a business plan may instead write a business plan for a relevant existing product in their area of interest.
Phase 2: Business/Medical Device idea Pitch (invitation only)
For those selected, you will submit and present a 15 to 20 minute business pitch of your idea in-person to the Fischell Foundry.
Upon acceptance into the fellowship, students are expected to also apply and be accepted into the M. Eng program.
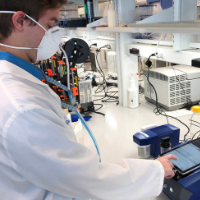
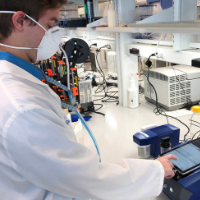
 Sam Meyr’s project focused on characterizing a 3D-printed bone scaffold for regulatory review and commercialization. These bone scaffolds can be customized to fit unique contours for patients and are composed of an allograft-based polymer. Meyr collaborated on this project with Eman Mirdamadi (BIOE Ph.D.’25) and member of BIOE professor Tao Lowe’s lab, who is leading similar research as part of his thesis. In addition to her bone scaffold project, Meyr assisted Fischell Institute Foundry engineers Ryan Smith and Kevin Aroom with projects within the institute.
Sam Meyr’s project focused on characterizing a 3D-printed bone scaffold for regulatory review and commercialization. These bone scaffolds can be customized to fit unique contours for patients and are composed of an allograft-based polymer. Meyr collaborated on this project with Eman Mirdamadi (BIOE Ph.D.’25) and member of BIOE professor Tao Lowe’s lab, who is leading similar research as part of his thesis. In addition to her bone scaffold project, Meyr assisted Fischell Institute Foundry engineers Ryan Smith and Kevin Aroom with projects within the institute.
Upon graduating the fellowship, Meyr joined Medtronic as an associate clinical specialist in technical support. Her responsibilities include troubleshooting cardiac devices, such as pacemakers and Implantable Cardioverter Defibrillators (ICDs). Meyr also provides engineering, sales, educational, and clinical support in response to field inquiries regarding cardiac rhythm management.
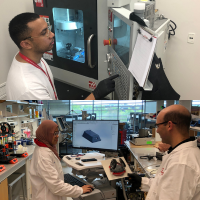
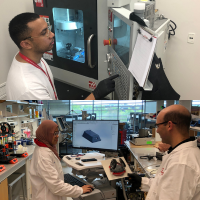
 Arsalan Siddiqui’s project focused on developing a circular surgical stapler for gastrointestinal anastomosis. Working closely with cardiothoracic surgeons, he aimed to redesign staple formation to improve reliability and tissue healing. The process involved mechanical design, prototyping and continual iteration. Siddiqui worked closely with clinicians and residents such as Aakash Shah, chief resident of cardiothoracic surgery at the University of Maryland Medical Center, to ensure the device met surgical needs. He also collaborated with the University of Maryland’s IP office to secure early patent protections and received support from engineers and prototyping specialists within the Fischell Institute to help troubleshoot and refine the design.
Arsalan Siddiqui’s project focused on developing a circular surgical stapler for gastrointestinal anastomosis. Working closely with cardiothoracic surgeons, he aimed to redesign staple formation to improve reliability and tissue healing. The process involved mechanical design, prototyping and continual iteration. Siddiqui worked closely with clinicians and residents such as Aakash Shah, chief resident of cardiothoracic surgery at the University of Maryland Medical Center, to ensure the device met surgical needs. He also collaborated with the University of Maryland’s IP office to secure early patent protections and received support from engineers and prototyping specialists within the Fischell Institute to help troubleshoot and refine the design.
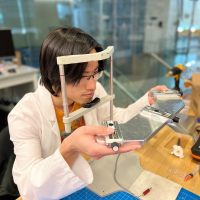
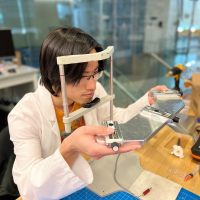
 Jason Chen worked with Fischell Institute Affiliate Fellow and bioengineering Assistant Professor Jenna Mueller to develop a triple-needle injector for ablating cervical pre-cancer in low-resource settings. The low-cost, repairable device employs a small air tank or bike pump to deliver three bolus doses of a drug or chemical mixture, such as ethyl cellulose ethanol. The injector was originally developed by MPower Fellow alumnus David Garvey. Chen also collaborated with Fischell Institute Director William Bentley and Fischell Institute Fellow and Institute for Bioscience and Biotechnology Research (IBBR) Research Professor Greg Payne on a potentiostat biosensor. The device monitors redox-active compounds, such as environmental pollutants or biotech products. Chen helped to functionalize and characterize printed circuit board-based electrodes and gather critical data to advance the biosensor’s capabilities.
Jason Chen worked with Fischell Institute Affiliate Fellow and bioengineering Assistant Professor Jenna Mueller to develop a triple-needle injector for ablating cervical pre-cancer in low-resource settings. The low-cost, repairable device employs a small air tank or bike pump to deliver three bolus doses of a drug or chemical mixture, such as ethyl cellulose ethanol. The injector was originally developed by MPower Fellow alumnus David Garvey. Chen also collaborated with Fischell Institute Director William Bentley and Fischell Institute Fellow and Institute for Bioscience and Biotechnology Research (IBBR) Research Professor Greg Payne on a potentiostat biosensor. The device monitors redox-active compounds, such as environmental pollutants or biotech products. Chen helped to functionalize and characterize printed circuit board-based electrodes and gather critical data to advance the biosensor’s capabilities.
 David Garvey’s research interest centers on cervical cancer, the fourth most common cancer among women worldwide. Women in low- and middle-income countries (LMICs) face disproportionately lower survival rates due to a variety of factors including limited access to trained providers and biomedical technologies needed to diagnose and treat cervical precancer before it becomes cancer.
David Garvey’s research interest centers on cervical cancer, the fourth most common cancer among women worldwide. Women in low- and middle-income countries (LMICs) face disproportionately lower survival rates due to a variety of factors including limited access to trained providers and biomedical technologies needed to diagnose and treat cervical precancer before it becomes cancer.
In 2021, Garvey and his fellow bioengineering Senior Capstone Design team members worked with Fischell Institute Affliate Fellow and Fischell Department of Bioengineering (BIOE) Assistant Professor Jenna Mueller to develop a handheld ethyl cellulose-ethanol (ECE) injector that could be used to treat precancerous lesions of the cervix. In order to deliver ECE to LMICs, the team proposed a low-cost, portable, handheld device that uses a rechargeable battery-powered injection system, a mechanical needle actuation system, and a dual needle design to decrease treatment time.
 As a computer science undergraduate, Jonathan Lin participated in UMD’s Gemstone Honors program – a unique, multidisciplinary, four-year research program for selected undergraduate Honors College students. Lin joined Team CONTACT – a group that worked to improve and lower the cost of glaucoma detection, a chronic disease of the eye linked to increased intraocular pressure that eventually results in blindness. Fischell Institute Fellow and BIOE Associate Professor Giuliano Scarcelli served as Team CONTACT’s mentor.
As a computer science undergraduate, Jonathan Lin participated in UMD’s Gemstone Honors program – a unique, multidisciplinary, four-year research program for selected undergraduate Honors College students. Lin joined Team CONTACT – a group that worked to improve and lower the cost of glaucoma detection, a chronic disease of the eye linked to increased intraocular pressure that eventually results in blindness. Fischell Institute Fellow and BIOE Associate Professor Giuliano Scarcelli served as Team CONTACT’s mentor.
Screening for glaucoma is most often conducted using what are known as tonometers, which focus on the accurate measurement of IOP. Existing non-contact tonometers forgo the use of probes and plungers. Team CONTACT worked to develop improved techniques for non-contact tonometry using deep neural networks, in conjunction with structured light projection, to calculate the movement of the entire corneal surface. Put simply, neural networks are the functional units of deep learning. They use a series of algorithms to mimic the way the human brain operates in order to solve complex problems.
 Quinn Burke worked to develop and enhance a conformal respirator mask alongside ActivArmor, a medical device company headquartered in Pueblo, Colo. Burke's work involves testing the respirators to meet U.S. Food and Drug Administration (FDA), National Institute for Occputational Safety and Health (NIOSH), and Occupational Safety and Health Administration (OSHA) standards. One of his goals is to scale up the manufacturing of these enhanced masks in Maryland. This project focuses on the continued translation of one of the projects initiated by the Fischell Institute’s COVID-19 response.
Quinn Burke worked to develop and enhance a conformal respirator mask alongside ActivArmor, a medical device company headquartered in Pueblo, Colo. Burke's work involves testing the respirators to meet U.S. Food and Drug Administration (FDA), National Institute for Occputational Safety and Health (NIOSH), and Occupational Safety and Health Administration (OSHA) standards. One of his goals is to scale up the manufacturing of these enhanced masks in Maryland. This project focuses on the continued translation of one of the projects initiated by the Fischell Institute’s COVID-19 response.
 Cio Defngin collaborated MPower fellow Ainul Wadhihah Abdul Rahim on producing the “Sleep Good Hood." The device aims to allow patients to rest comfortably at night without impeding necessary ICU workflow (nurses/doctors performing intubation, diagnostics, etc). Their clinical mentor is Jeffrey Hasday, Professor of Medicine, Pathology and Biochemistry & Molecular Biology, Head of the Pulmonary and Critical Care Medicine Division at the University of Maryland School of Medicine.
Cio Defngin collaborated MPower fellow Ainul Wadhihah Abdul Rahim on producing the “Sleep Good Hood." The device aims to allow patients to rest comfortably at night without impeding necessary ICU workflow (nurses/doctors performing intubation, diagnostics, etc). Their clinical mentor is Jeffrey Hasday, Professor of Medicine, Pathology and Biochemistry & Molecular Biology, Head of the Pulmonary and Critical Care Medicine Division at the University of Maryland School of Medicine.
 Rayan Alabsi and Tejasvi Subramanya developed the prototype for a novel reverse shoulder implant they hope could change the way shoulder surgeries are done.
Rayan Alabsi and Tejasvi Subramanya developed the prototype for a novel reverse shoulder implant they hope could change the way shoulder surgeries are done.
The pair’s prosthesis is designed for patients undergoing Reverse Total Shoulder Arthroplasty (RTSA), the surgical reconstruction and replacement of the shoulder. The damaged shoulder joint is replaced with a prosthesis, with the anatomical ball and socket joint reversed. RTSA is a relatively new surgery; it was approved by the U.S. Food and Drug Administration (FDA) in 2003.
Alabsi and Subramanya were inspired to design a RTSA-specific device because of the rising number of people undergoing the surgery every year. Despite the increase in patients, numerous challenges in prosthesis design, biomechanics positioning, and surgical techniques are still associated with the surgery. Alabsi and Subramanya's device consists of mechanical features which allow for a larger range of motion and significantly smaller risk of joint dislocation and reduction of scapular bone impingement compared with other devices.
 Alex Woo’s fellowship project was continuing his BIOE undergraduate Capstone project, focused on a bedside sputum analysis system. Sputum is monitored by physicians to inform decisions about starting, stopping, and even modifying therapies for patients with acute and chronic lung diseases. These pulmonary diseases include COPD, chronic asthma, and cystic fibrosis. Sputum changes are an important indicator of success or failure of treatment for respiratory infections. The physical characteristics of sputum are an important consideration when deciding whether patients are ready for removal of endotracheal tubes. However, current practice is limited to qualitative measures by nurses, respiratory therapists, and (in the outpatient setting), patients themselves.
Alex Woo’s fellowship project was continuing his BIOE undergraduate Capstone project, focused on a bedside sputum analysis system. Sputum is monitored by physicians to inform decisions about starting, stopping, and even modifying therapies for patients with acute and chronic lung diseases. These pulmonary diseases include COPD, chronic asthma, and cystic fibrosis. Sputum changes are an important indicator of success or failure of treatment for respiratory infections. The physical characteristics of sputum are an important consideration when deciding whether patients are ready for removal of endotracheal tubes. However, current practice is limited to qualitative measures by nurses, respiratory therapists, and (in the outpatient setting), patients themselves.
The goal of Woo’s project was to develop a user-friendly sputum collection system and a bedside or benchtop device that will quickly, reproducibly, and objectively provide quantitative data for physicians to evaluate. This data included the viscosity, elasticity, and color of the sputum sample. The quantitative and reproducible information provided to the physicians will improve decision-making about patient management as well as provide a discrete outcome for clinical studies of disease intervention.
 Negeen Haghighi’s fellowship project was a continuation of her BIOE Capstone project. Her project focused on a simple way to ensure that automated feeding pumps are properly used to maximize nutritional intake in patients in the ICU. Proper nutritional intake is critical to help prevent muscle atrophy. Muscle atrophy is the loss of muscle tissue due to the lack of protein in the body and can affect up to 90 percent of critically ill patients in the ICU. Decreased muscle mass can significantly impact the rehabilitation time of a patient after hospitalization.
Negeen Haghighi’s fellowship project was a continuation of her BIOE Capstone project. Her project focused on a simple way to ensure that automated feeding pumps are properly used to maximize nutritional intake in patients in the ICU. Proper nutritional intake is critical to help prevent muscle atrophy. Muscle atrophy is the loss of muscle tissue due to the lack of protein in the body and can affect up to 90 percent of critically ill patients in the ICU. Decreased muscle mass can significantly impact the rehabilitation time of a patient after hospitalization.
The primary factors that lead to muscle atrophy are insufficient protein intake and reduced muscle use. One main cause of insufficient caloric intake is linked to errors and inaccuracies that arise when determining the correct placement of the feeding tube and the proper flow rate of the food. Currently, feeding tube flow rates are adjusted manually based on a feeding schedule and pump flow rate chart.
The manual adjustment process can allow for human error and miscalculation of the flow rate including an insufficient amount of food. Conversely too fast of a flow rate can cause vomiting or bloating due to overfilling and a built-up pressure in the patient’s stomach. Current feeding schedules do not take into account when a patient is disconnected from the continuous feeding tube and so commonly patients have nutritional insufficiencies.
 Sam Meyr’s project focused on characterizing a 3D-printed bone scaffold for regulatory review and commercialization. These bone scaffolds can be customized to fit unique contours for patients and are composed of an allograft-based polymer. Meyr collaborated on this project with Eman Mirdamadi (BIOE Ph.D.’25) and member of BIOE professor Tao Lowe’s lab, who is leading similar research as part of his thesis. In addition to her bone scaffold project, Meyr assisted Fischell Institute Foundry engineers Ryan Smith and Kevin Aroom with projects within the institute.
Sam Meyr’s project focused on characterizing a 3D-printed bone scaffold for regulatory review and commercialization. These bone scaffolds can be customized to fit unique contours for patients and are composed of an allograft-based polymer. Meyr collaborated on this project with Eman Mirdamadi (BIOE Ph.D.’25) and member of BIOE professor Tao Lowe’s lab, who is leading similar research as part of his thesis. In addition to her bone scaffold project, Meyr assisted Fischell Institute Foundry engineers Ryan Smith and Kevin Aroom with projects within the institute.



 As a computer science undergraduate, Jonathan Lin participated in UMD’s Gemstone Honors program – a unique, multidisciplinary, four-year research program for selected undergraduate Honors College students. Lin joined Team CONTACT – a group that worked to improve and lower the cost of glaucoma detection, a chronic disease of the eye linked to increased intraocular pressure that eventually results in blindness. Fischell Institute Fellow and BIOE Associate Professor
As a computer science undergraduate, Jonathan Lin participated in UMD’s Gemstone Honors program – a unique, multidisciplinary, four-year research program for selected undergraduate Honors College students. Lin joined Team CONTACT – a group that worked to improve and lower the cost of glaucoma detection, a chronic disease of the eye linked to increased intraocular pressure that eventually results in blindness. Fischell Institute Fellow and BIOE Associate Professor