News Story
Combating Metastatic Cancer Through Blood Draw
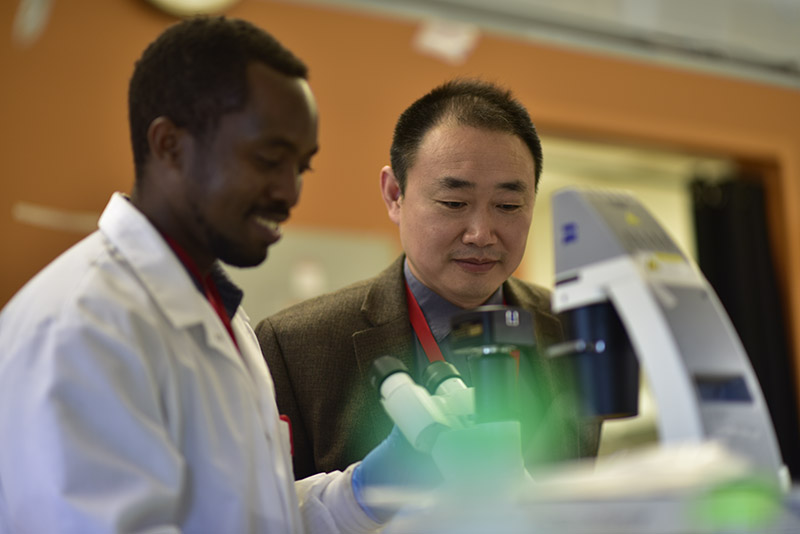
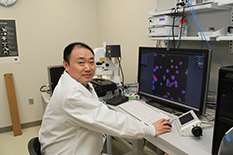
Drs. Elyahb A. Kwizera and Xiaoming (Shawn) He. Photo courtesy of Alan P. Santos (University of Maryland).
University of Maryland bioengineers have developed a new technique to capture, release, scale up, and analyze circulating tumor cells, one of the primary culprits in metastatic cancer. The group’s hope is that their approach can be used to understand why and how certain cancers spread and that resulting findings could one day lead to new personalized therapeutic options.
The vast majority of cancer deaths result from metastasis, whereby tumor cells break away from a primary tumor, enter the bloodstream, and form a new tumor in a distant organ or tissue. These breakaway tumor cells are known as circulating tumor cells (CTCs), and they represent just a tiny population of cancer cells in the blood – in fact, there are typically fewer than one CTC per 1 million white blood cells.
Scientists first discovered CTCs in the late 19th century, and yet there is still little known about why some CTCs survive the arduous journey through the bloodstream better than others, or why some go on to form secondary tumors that are highly resistant to treatment.
This knowledge gap is partially because there are so few CTCs in the blood, so scientists and clinicians need a way to isolate and culture – or grow more – CTCs outside the body in order to have enough for analysis.
As it turns out, culturing CTCs outside the body – in vitro – is incredibly difficult to do.
 “The biggest challenge for CTC research is the rarity of CTCs in the blood,” said Elyahb A. Kwizera, a University of Maryland Fischell Department of Bioengineering (BIOE) researcher and co-lab manager of BIOE Professor Xiaoming (Shawn) He’s Multiscale Biomaterials Engineering Laboratory. “Capturing this small number of cells from the bloodstream requires some sensitive technologies that can efficiently fish these cells from millions of other blood cells. Moreover, with this tiny number of cells, it is very challenging to do any downstream analysis. Developing a technology with the capability of efficient capture, release, and culture to increase the number of CTCs will help researchers better understand CTCs and their role in metastasis. Even more, this technology could also help researchers identify ways in which CTCs could be used to design personalized therapies for patients.”
“The biggest challenge for CTC research is the rarity of CTCs in the blood,” said Elyahb A. Kwizera, a University of Maryland Fischell Department of Bioengineering (BIOE) researcher and co-lab manager of BIOE Professor Xiaoming (Shawn) He’s Multiscale Biomaterials Engineering Laboratory. “Capturing this small number of cells from the bloodstream requires some sensitive technologies that can efficiently fish these cells from millions of other blood cells. Moreover, with this tiny number of cells, it is very challenging to do any downstream analysis. Developing a technology with the capability of efficient capture, release, and culture to increase the number of CTCs will help researchers better understand CTCs and their role in metastasis. Even more, this technology could also help researchers identify ways in which CTCs could be used to design personalized therapies for patients.”
For years, scientists and clinicians have relied on a capture technique that zeroes in on a marker displayed by many tumor cells, including many breast cancer malignancies. By targeting this marker – an antibody known as the epithelial cell adhesion molecule (EpCAM) – scientists can capture CTCs from patients’ blood for cancer detection, prognosis, and research.
But, CTCs – like their “parent” cancer cells found in the primary tumor – are actually quite complex. CTCs are very heterogeneous; they can have different morphologies and genetic characteristics, and each may contribute differently to metastasis or cancer drug resistance.
CTCs may also go through an evolutionary process of sorts whereby they no longer express EpCAM or other epithelial markers. This, of course, represents a major weakness when scientists and clinicians rely on EpCAM capturing to collect CTCs. To add another layer of difficulty, researchers run into major roadblocks when they try to culture captured CTCs in vitro after using this method.
“Capturing CTCs using EpCAM alone misses the heterogeneity of CTCs,” He said. “Treatments that are developed based on EpCAM-captured CTCs may lack the ability to kill CTCs that no longer express EpCAM. Even worse, EpCAM-captured CTCs from only 3 to 16 percent of stage 4 breast cancer patients can be successfully cultured to proliferate in vitro. This means that for more than 80 percent of stage 4 breast cancer patients – who usually have metastasis – their CTCs couldn’t be grown and scaled up for the development of patient-specific targeted therapies. This is disappointing and needs to be addressed.”
For the majority of patients with stage 4 cancer today, key information to guide their treatment is most often obtained from surgical tumor biopsies; in some cases, this tumor tissue could be several years old and may not reflect the current tumor sensitivities to therapies.
"Developing a technology with the capability of efficient capture, release, and culture to increase the number of CTCs will help researchers better understand CTCs and their role in metastasis," said Fischell Department of Bioengineering researcher Elyahb A. Kwizera. "Even more, this technology could also help researchers identify ways in which CTCs could be used to design personalized therapies for patients."
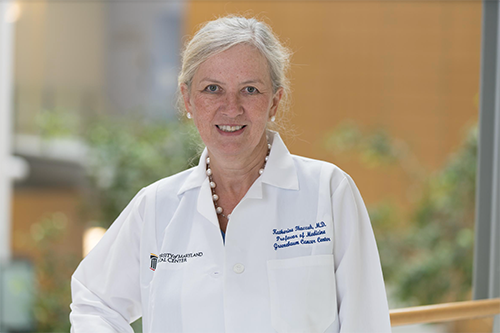 “A new tumor biopsy can provide access to cancer cells but often the amount of tissue is small and may limit the ability to perform certain tests for tumor targets that are crucial in determining which cancer treatment will have the best antitumor effect,” said Katherine Tkaczuk, M.D., Director of the University of Maryland School of Medicine Marlene and Stewart Greenebaum Cancer Center’s (UMGCCC) Breast Evaluation and Treatment Program. “Having access to ‘fresh,’ current cancer cells such as the CTCs provides much-needed access to the tumor cells, which then are tested for specific targets for therapy.”
“A new tumor biopsy can provide access to cancer cells but often the amount of tissue is small and may limit the ability to perform certain tests for tumor targets that are crucial in determining which cancer treatment will have the best antitumor effect,” said Katherine Tkaczuk, M.D., Director of the University of Maryland School of Medicine Marlene and Stewart Greenebaum Cancer Center’s (UMGCCC) Breast Evaluation and Treatment Program. “Having access to ‘fresh,’ current cancer cells such as the CTCs provides much-needed access to the tumor cells, which then are tested for specific targets for therapy.”
Recognizing these challenges, Kwizera, He, Tkaczuk, and a team of researchers set out to develop a new technique to capture and scale up CTCs in vitro. Their goal is to advance understanding of how and why cancers metastasize so that new targeted personalized cancer therapies could be developed to tackle hard-to-treat cancers.
“The clinical translational studies we are currently conducting are utilizing breast cancer patients’ samples for isolation of CTCs to provide a more accurate and up-to-date glimpse into patients’ tumors and ultimately improve cancer treatment outcomes by utilizing more personalized targeted anticancer therapies,” Tkaczuk said.
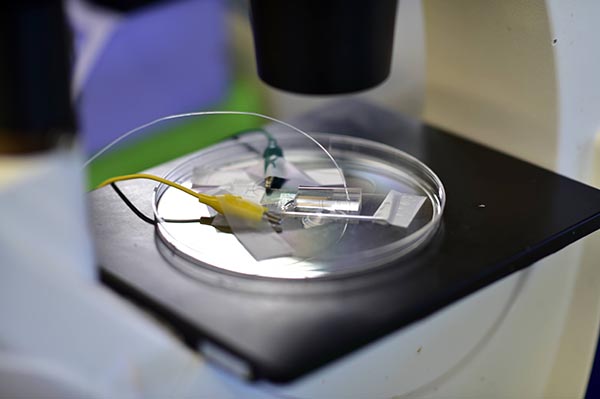 At the focal point of the team’s work is a microfluidic chip they call VIZA, which is short for “virtually implemented zones surface-coated with gold (noted by the chemical symbol Au).” To capture their CTCs, they work not only with EpCAM, but also with a second antibody – known as CD44 – which is one of the most common cancer stem cell markers and a promising prognostic biomarker for many malignancies, including breast cancer.
At the focal point of the team’s work is a microfluidic chip they call VIZA, which is short for “virtually implemented zones surface-coated with gold (noted by the chemical symbol Au).” To capture their CTCs, they work not only with EpCAM, but also with a second antibody – known as CD44 – which is one of the most common cancer stem cell markers and a promising prognostic biomarker for many malignancies, including breast cancer.
Why exactly VIZA’s special combination of a gold layer and electromicrofluidic technology works is complex, but so far the device has produced exciting results. He and Kwizera’s team has successfully demonstrated that VIZA can be conveniently modified with EpCAM alone, CD44 alone, or a combination of CD44 and EpCAM to capture a tiny number of CTCs from a blood sample. Even more, the group successfully cultured those CTCs in vitro for stage 4 breast cancer patients – a major milestone for advancing the study of metastatic cancers and targeted personalized cancer therapy.
For years, researchers have always focused on CTC capture and in vitro culture using EpCAM alone, despite the fact that few EpCAM-captured CTCs can grow in in vitro culture.
“The exciting news is that our team has shown that CTCs captured by either the combination of CD44 and EpCAM or CD44 alone from up to approximately 70 percent of stage 4 breast cancer patients can grow in culture,” Elyahb said.
“The capability of culturing CTCs to scale them up in vitro is invaluable, as it creates a large enough supply of CTCs to enable analysis of their gene and protein expression,” He said. “This is critical for identifying patient-specific targets and for building CTC-based tumor models for patient-specific drug screening. Eventually, this may enable the development of targeted, personalized therapies for curing hard-to-treat metastatic cancers.”
Notably, this CTC-based pathway for therapeutic development is both convenient and safe: it can be carried out via a routine blood draw. Conversely, the conventional pathway relies on an intratumoral biopsy, which is often very difficult to do for distant metastases, He noted.
The group’s breakthrough findings were published earlier this month in ACS Nano under the title “Greatly Enhanced CTC Culture Enabled by Capturing CTC Heterogeneity Using a PEGlyated PDMS-Titanium-Gold Electromicrofluidic Device with Glutathione-Controlled Gentle Cell Release.”
Elyahb A. Kwizera served as first author of the ACS Nano paper. Xiaoming (Shawn) He and Katherine Tkaczuk, M.D. served as co-corresponding authors. BIOE postdoctoral researchers Wenquan Ou and Jiangsheng Xu, BIOE graduate students Samantha Stewart (BIOE) and James G. Shamul (BIOE), and UMGCCC research coordinator Nancy Tait also contributed to the paper.
In addition to his appointment as BIOE professor, He also holds affiliations with UMGCCC as well as with the University of Maryland’s Robert E. Fischell Institute for Biomedical Devices.
Published July 20, 2022