News Story
Fischell Institute and Children’s National Collaborate to Develop Pediatric Tracheostomy Safety Device

The Robert E. Fischell Institute for Biomedical Devices is working with Jules Sherman, director of the Biodesign Program at Children’s National Hospital and adjunct professor in the Fischell Department of Bioengineering at the University of Maryland, to develop Trach Sense, a device that monitors breathing for children with tracheostomies.
A tracheostomy is an opening created surgically through the neck into the trachea (windpipe) that allows air to fill the lungs. After creating the opening, surgeons insert a tube through it to create an airway and create a path to remove secretions from the lungs. Patients receiving a tracheostomy breathe through the tube rather than through the nose and mouth, either temporarily or permanently.
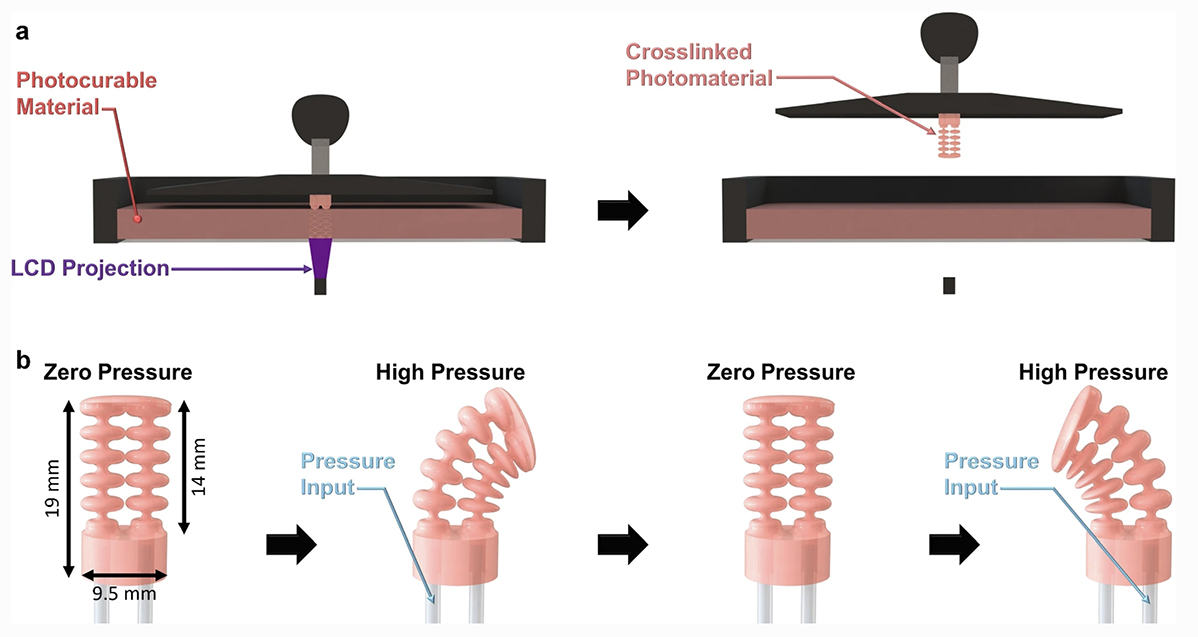
Trach Sense is a capnograph device that sits atop pediatric tracheostomy tubes to continuously monitor carbon dioxide levels via waveforms. The device is intended to keep children safe by immediately alerting caregivers if the tube becomes blocked or dislodged.
“For children with trachs, ventilation issues can arise suddenly and often silently,” said Sherman. “Right now, there's no simple, continuous way to monitor breathing for children with a trach tube who are not ventilator dependent. Our goal was to create a solution that brings critical insight to both long-term and home care settings, giving clinicians and caregivers peace of mind and more time to act when something goes wrong.”
Trach Sense was first developed as part of a student-led project in the Fischell Department of Bioengineering, where MPower Fellow Arsalan Siddiqui led the initial design, sensor selection, technical specifications, and early bench testing in collaboration with Sherman and additional student team members.
Sherman then brought the prototype to the Fischell Institute Foundry to refine the device and prepare it for clinical testing.
Foundry Engineer Quinn Burke designed and constructed a breathing circuit for the initial testing of the device. This custom setup used a pediatric breathing simulator and 3D-printed trachea models developed by researchers at Memorial University of Newfoundland, representing 0 to 3 months of age, a 2 to 4 year old, and a 10 to 12 year old.
Burke and Siddiqui then collaborated on validation testing efforts for Trach Sense, assessing the device’s accuracy, responsiveness, and reliability under simulated clinical conditions. Their work played a critical role in refining the system for real-world use, and later led to a study published in Tracheostomy: Official Journal of the Global Tracheostomy Collaborative, a peer-reviewed journal, on the device’s performance.
Following the initial testing, Burke worked alongside Fischell Foundry Chief Engineer John Rzasa to miniaturize the system and integrate Bluetooth communication for real-time wireless monitoring. Rzasa also redesigned the device’s printed circuit boards to improve signal processing and carbon dioxide measurement, while decreasing the size of the housing and making it battery powered.
The device identifies two serious events: tube obstruction and accidental removal. It does this by monitoring end-tidal carbon dioxide levels and analyzing waveform patterns. A blockage results in altered waveforms, while complete decannulation causes a flatline.
Integrating Bluetooth on the device offers caregivers peace of mind knowing they can be immediately notified via a mobile application if the tube has become blocked or dislodged, both somewhat common, potentially life-threatening occurrences in pediatric patients with trach tubes.
To this end, Foundry engineers enlisted help from students in the University of Maryland’s App Development Club to create a mobile app that connects to the device, providing real-time alerts. The interface was designed with feedback from nurses to ensure accessibility for nonmedical users. With the help of the app and an onboard Wi-Fi hub extending the system’s reach, caregivers are able to receive alerts even when away from the child.
“It brings ICU-level monitoring into settings where that level of surveillance isn’t typically available,” said Sherman. ”We want families to feel more secure, knowing they have an early warning system watching over their child, and we want clinicians to have better tools for monitoring vulnerable patients without relying solely on high-resource settings. Ultimately, it’s about giving every child with a trach a safer future.”
Additional guidance was provided by Children’s National clinicians Rahul Shah and Habib Zalzal, who helped identify clinical needs and supported development efforts.
"The Fischell Institute has been instrumental in translating clinical insight into an engineered solution,” Sherman added. “Their team brought the technical expertise to prototype, iterate, and refine the device alongside our clinical partners—it has been a true collaboration between qualitative research, medicine and engineering. Our hope is that Trach Sense becomes a safety net for children with trachs, whether they are in a long-term care facility or living their best mobile life."
The team is finalizing the device’s design and mobile application, and plans to conduct a pilot study with Children’s National Hospital.
Published August 13, 2025