News Story
Cancer in the Crosshairs

For more than a century, the medical community has tapped vaccines to treat a wide variety of diseases, from smallpox and the flu, to HIV, and, most recently, COVID-19. But, recent findings – as well as advanced understanding of how the human immune system functions – have enabled bioengineers to zero in on a high-priority target: cancer.
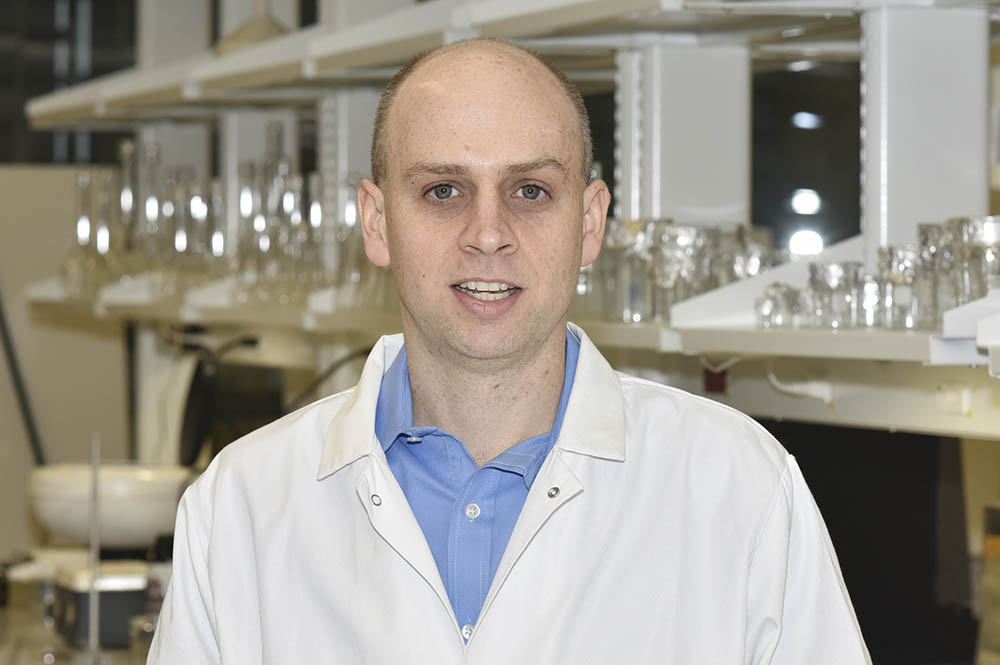
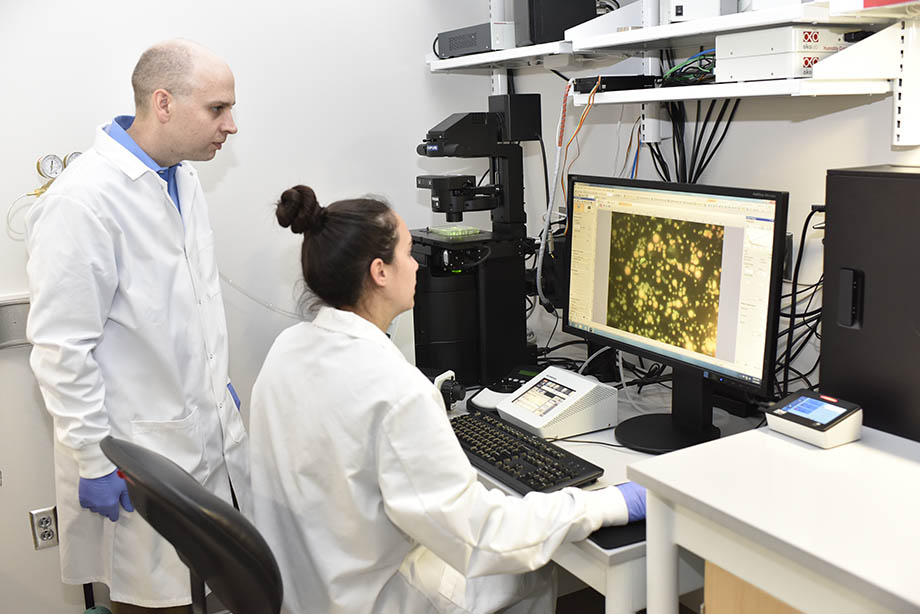
At the University of Maryland (UMD), MPower Professor and Minta Martin Professor of Engineering Christopher M. Jewell and members of his Immune Engineering Lab are taking cancer vaccine development to the next level by developing new techniques to tailor the body’s immune response to cancer. The group is working to design vaccines that carry new therapy combinations in order to coax the immune system to recognize, attack, and prevent recurrence of cancer – all without harming nearby healthy cells. The group’s most recent findings were published this week in Advanced Science.
“As we’ve seen from the pandemic, in cancers, and many other diseases, a key goal for next-generation vaccines and immunotherapies is the ability to quickly design these tools to tailor immunity for evolving pathogens or specific individuals,” Jewell said. “Stimulatory molecules – adjuvants – play a fundamental role in these processes.”
Overcoming a Roadblock
Traditionally, vaccines work by exposing the body to antigens – molecules that can trigger a specific immune response. The antigens carried by vaccines mimic, or are fragments of, pathogens – a bacterium, virus, or other microorganism that causes disease. Additionally, vaccines carry stimulatory signals – adjuvants – that help the immune system generate large responses against antigens. With both components, vaccines can mimic a specific pathogen in order to stimulate the body’s immune system to build up defenses against disease agents.
In recent years, bioengineers have studied the use of biomaterials as vaccine carriers, as they offer advantages such as controlled release of the vaccine, targeting, and “cargo” protection; however, biomaterials-based vaccines present a number of challenges, too.
To start, biomaterials carriers often contain components that can activate the immune system by themselves in ways unintended. This means that, even if one knows what to expect from a certain vaccine, he or she may find that the biomaterials used as carriers alter the immune response triggered by the vaccine. As a result, vaccines that offer promising treatment or cures for diseases might not have the same effects as predicted because the carrier itself alters the response to the antigens. Further, this challenge – one shared by all vaccines – makes understanding how existing and new vaccines work difficult because the role of each individual component to the vaccine’s overall effectiveness is unclear.
Recognizing these obstacles, Jewell and his team have developed simplified vaccines by assembling immune signals in ways that eliminate the need for traditional biomaterials while maintaining their useful features, such as co-delivery.
Precision Control of Immune Function
 When it comes to any disease, the body’s ability to fight infection depends on factors beyond antigens. For example, in cancers, the cancer cells themselves create microenvironments that actively suppress the body’s antitumor immune response. Due to these factors, it’s often a toss-up whether the immune system will support or inhibit tumor occurrence, spread, or relapse.
When it comes to any disease, the body’s ability to fight infection depends on factors beyond antigens. For example, in cancers, the cancer cells themselves create microenvironments that actively suppress the body’s antitumor immune response. Due to these factors, it’s often a toss-up whether the immune system will support or inhibit tumor occurrence, spread, or relapse.
Knowing this, Jewell and his team are working to design vaccines that enable precision control of multiple immune signaling pathways to tailor the body’s immune response. Among these are what are known as toll-like receptors (TLRs), a class of proteins that plays a key role in mediating the body’s immune response.
To harness the power of TLRs without inducing unwanted immune responses, Jewell and his team developed polyelectrolyte multilayer (PEM) vaccine coatings built entirely from immune signals. These immune-PEMs (iPEMS) are self-assembled on nanoparticle templates during production. Then, the templates are dissolved to leave hollow micro- or nano-capsules that consist only of the cues the researchers want to deliver, concentrating these signals to drive potent and precise responses.
In their Advanced Science paper, Jewell and his team report a new discovery that self-assembly of combinations of these important immune cues drives potent responses that can be directed toward completely different outcomes, depending on the combination of TLR adjuvant molecules. This ability could allow plug-N-play type technologies for quickly designing or modifying vaccines or immunotherapies.
So far, the research team’s findings are promising. In mouse models, Jewell and his group demonstrated that by activating multiple TLR pathways with iPEM vaccination they could increase the frequency, trafficking, and proliferation of antigen-specific T cells, a type of immune cell that is uniquely effective at infiltrating tumors.
“This was a really exciting story for us,” Jewell said. “When we discovered that iPEMs sequestered TLRs to the vaccine capsules in immune cells, we wondered if it might allow selective activation of specific immune pathways. We started probing this and discovered that we could make completely different types of immune responses to a given antigen by assembling different combinations of adjuvants. Perhaps most importantly, we found that using this platform to activate sets of stimulatory immune pathways gave synergistic response during disease, such as in preclinical cancer models.”
University of Maryland Fischell Department of Bioengineering (BIOE) alum Michelle Bookstaver (Ph.D. ‘21) served as first author of the Advanced Science paper titled “Self-Assembly of Immune Signals to Program Innate Immunity through Rational Adjuvant Design.” Along with Bookstaver and Jewell, the following Jewell Lab researchers contributed to the paper: Qin Zeng (former BIOE postdoc), Robert “Smitty” Oakes (BIOE postdoc), Senta Kapnick (BIOE assistant research scientist), Camilla Edwards (BIOE Ph.D. candidate), Nishedhya Venkataraman (UMD neuroscience undergraduate student), Sheneil K. Black (BIOE faculty specialist), Xiangbin Zeng (former Jewell Lab manager), and Eugene Froimchuk (BIOE Ph.D. candidate). Jonathan S. Bromberg, M.D., and Vikas Saxena of the University of Maryland School of Medicine also contributed to this research, along with Thomas Gebhardt of the University of Melbourne at the Peter Doherty Institute for Infection and Immunity.
In addition to his primary appointment in the Fischell Department of Bioengineering, Jewell is also a UMD Robert E. Fischell Institute for Biomedical Devices Fellow and a research biologist with the U.S. Department of Veterans Affairs.
This work was supported in part by the National Institutes of Health, the U.S. Department of Veterans Affairs, the Damon Runyon Foundation, the Alliance for Cancer Gene Therapy, the Melanoma Research Alliance, and the National Science Foundation. Jewell holds an equity position with Vaccitech plc.
Published November 16, 2022